By the end of this article, you’ll have the perfect AI progress note generator that can create highly accurate progress notes—for free!
It all started with a simple idea!
What if we could take the load off healthcare professionals so they can focus more on patients and less on paperwork?
With the most advanced algorithms and machine learning, this tool has already helped thousands of professionals get more productive by enabling them to generate accurate progress notes quickly and efficiently!
So why not give it a try? After all, what have you got to lose—except maybe those stacks of paperwork.
Key Takeaways
- Download Jamie and set up your customized templates.
- Start using Jamie during your next session to see immediate benefits.
- Save and share your notes with ease, and enjoy more time to focus on patient care.
How Can Jamie Help Automate Your Soap and Dap Notes?
As healthcare professionals deal with many patients, it is hard to keep track and often miss crucial information or, at worst, mix information, which could lead to critical errors.
And in the medical field, there is absolutely “no room for errors.”
“And with Jamie, there’s truly no room for error.”

Jamie is a free AI tool that helps you quickly generate progress notes like SOAP, DAP, and even full treatment plans.
By making the process of creating progress notes more efficient, Jamie, a progress notes software, assists therapists, consultants, and other healthcare professionals in becoming more organized and efficient—because when it comes to paperwork, who wouldn’t want a prescription for precision?
Here’s How Jamie Can Help You With Your Progress Notes
- Executive Assistant Sidebar: Acts as a ChatGPT right next to your screen.
- No Bots for Quiet Meetings: Keeping your consultation private and confidential
- Very Detailed Notes: Captures every detail with the greatest accuracy.
- Wide Compatibility: Works with any video conferencing platform.
- Customization for Your Needs: Customize templates and train Jamie to know your medical terms.
- Data Safety and Privacy: Encrypted and GDPR compliant and audio deleted after transcription.
- Speaker Identification: It identifies who said what in meetings.
- Offline Note Capture: It takes notes even without the internet.
- Diversity: Jamie can transcribe in over 15 languages and understand different accents.
- Instant Share: Share notes instantly via email or a secure URL.
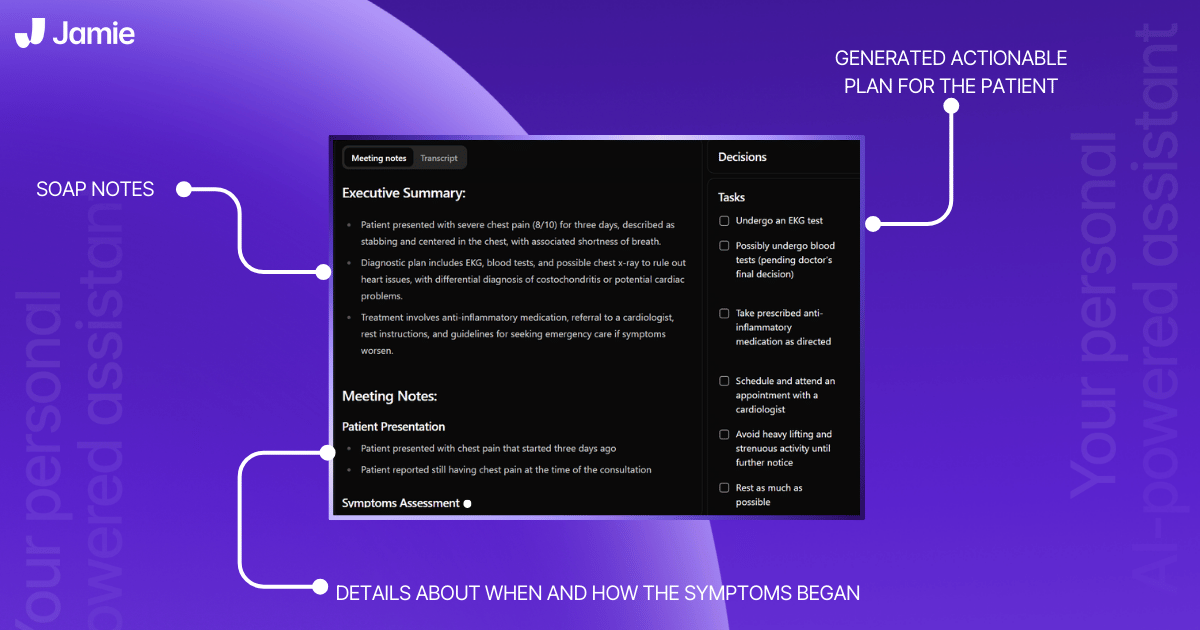
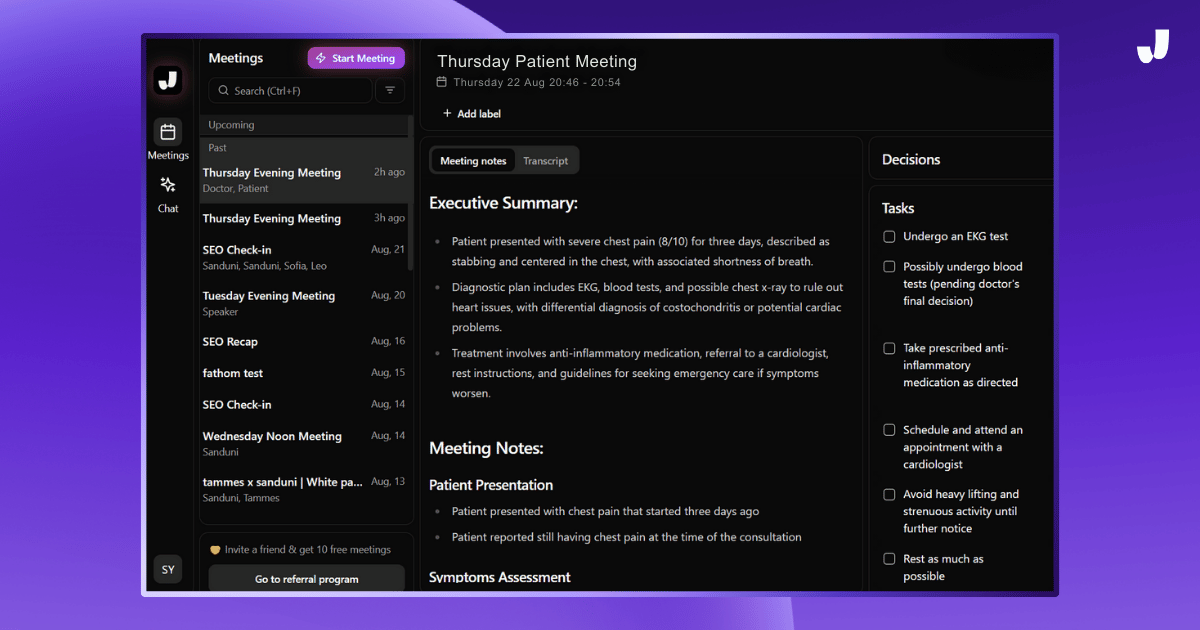
Here is a real-life meeting note taken using Jamie's progress note-taking method.
Step-by-Step Guide: How Jamie Helps
Quick Start
Install Jamie > Settings > Summary > Add New Template > Customize Your Template > Start Your Meeting > Choose a Template > Let Jamie Handle the Rest
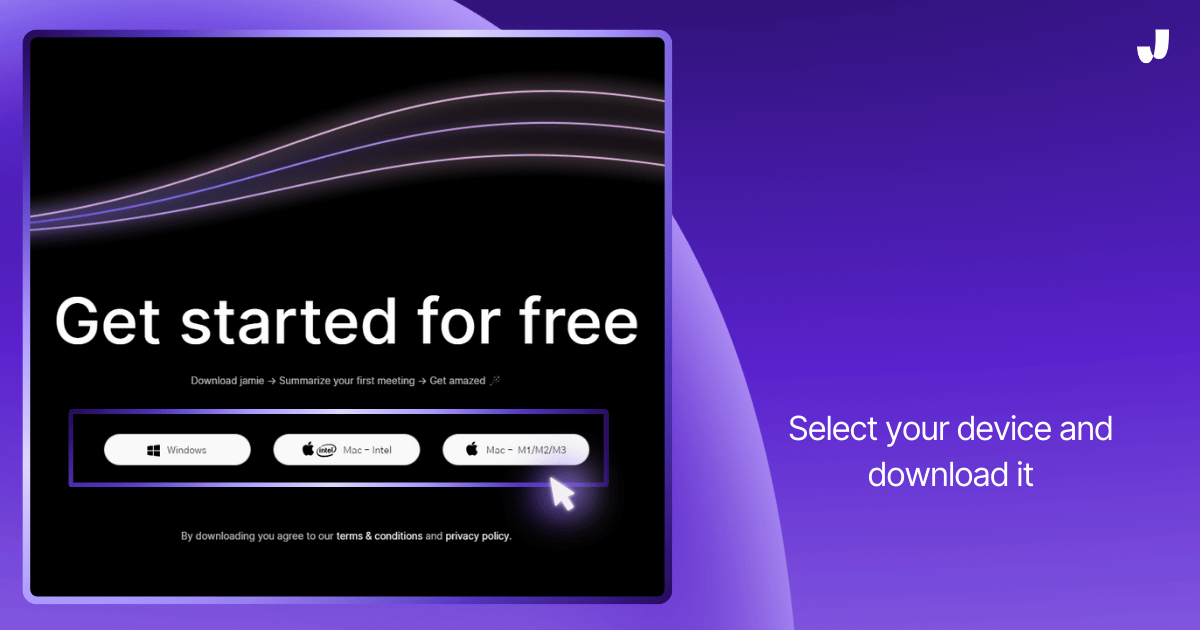
Step 1: Download Jamie First
Download Jamie from the official website and install it on your device.
Step 2: Open Jamie Once Jamie is Installed
Step 3: Go to Settings
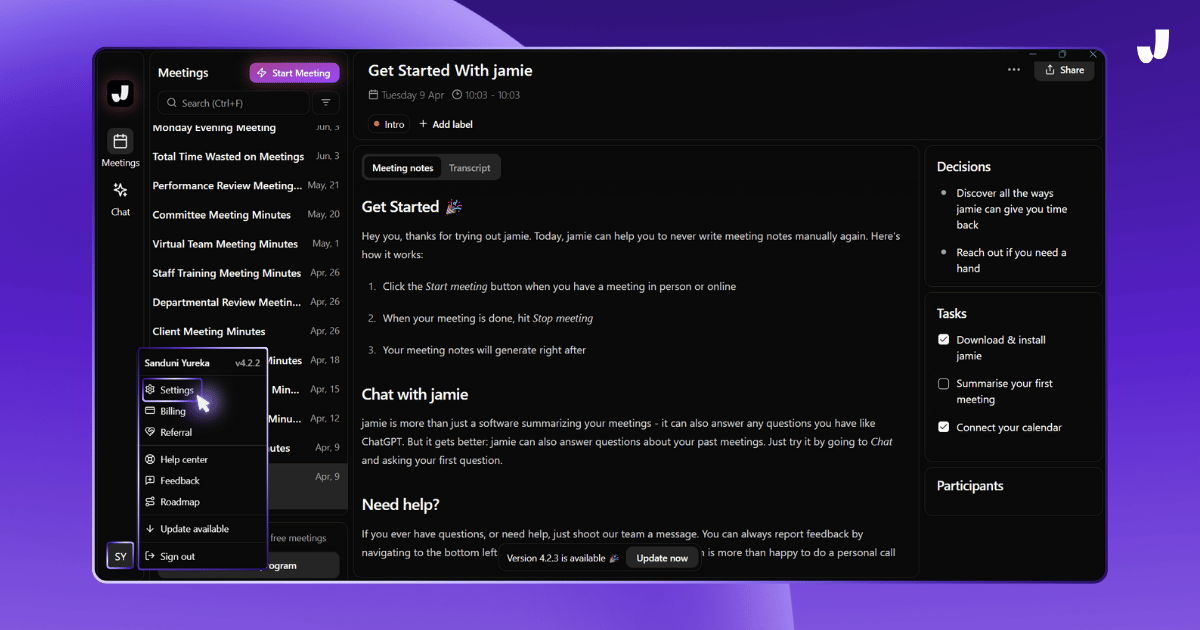
Step 4: Navigate to General > Summary In the settings
Go to the “General” section and in the "Summary" menu, you will see "Add new template."
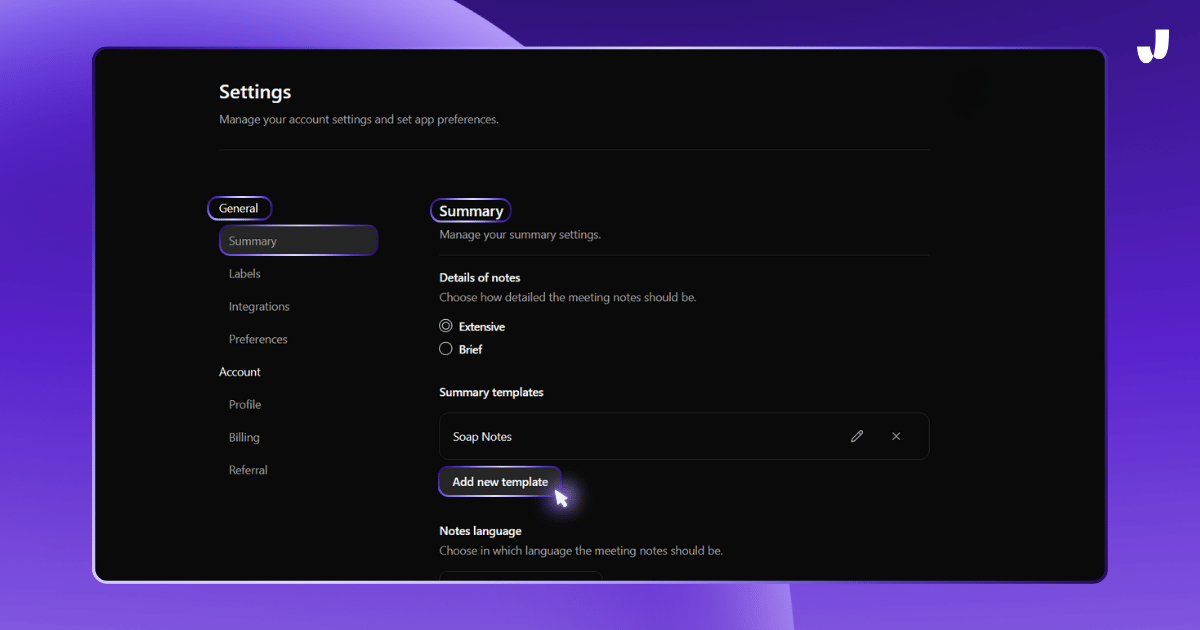
This is where you can customize how Jamie will summarize your meetings.
Step 5: Add a New Template
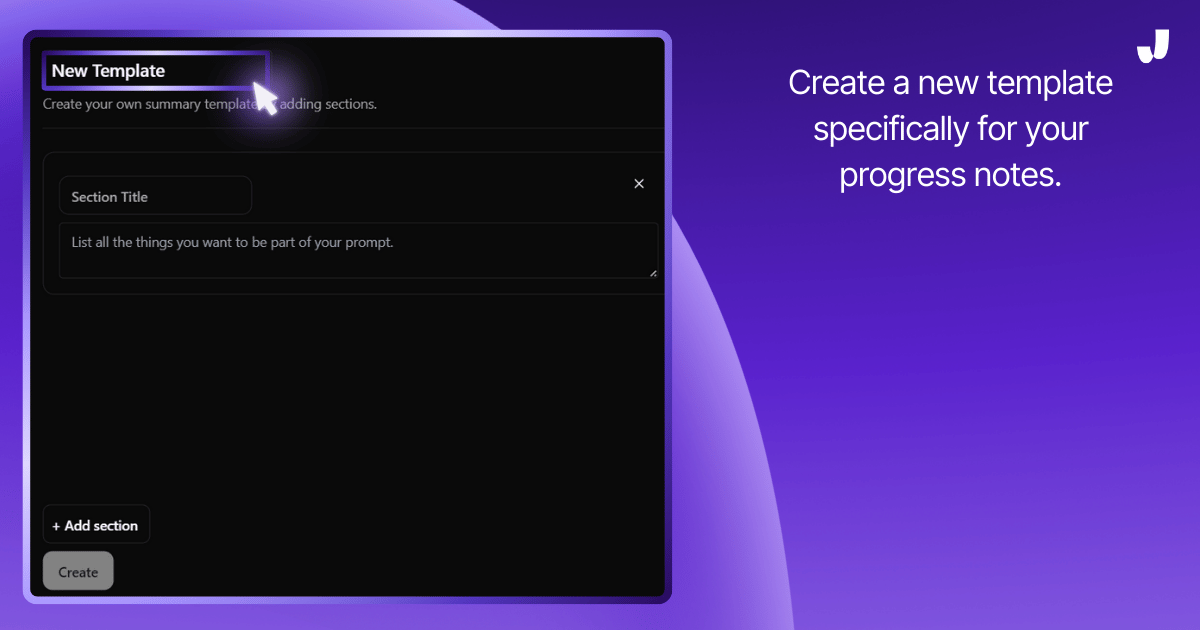
Create a new template specifically for your progress notes. You can choose to set it up for SOAP, DAP, or any other format you prefer. This makes it ideal for generating notes for physical therapy, occupational therapy, or speech therapy.
Step 6: Customize Your Template
Now that you’ve added a new template, it’s time to customize it for your needs:
- Template Title: Start by naming your template. In this case, name it SOAP.
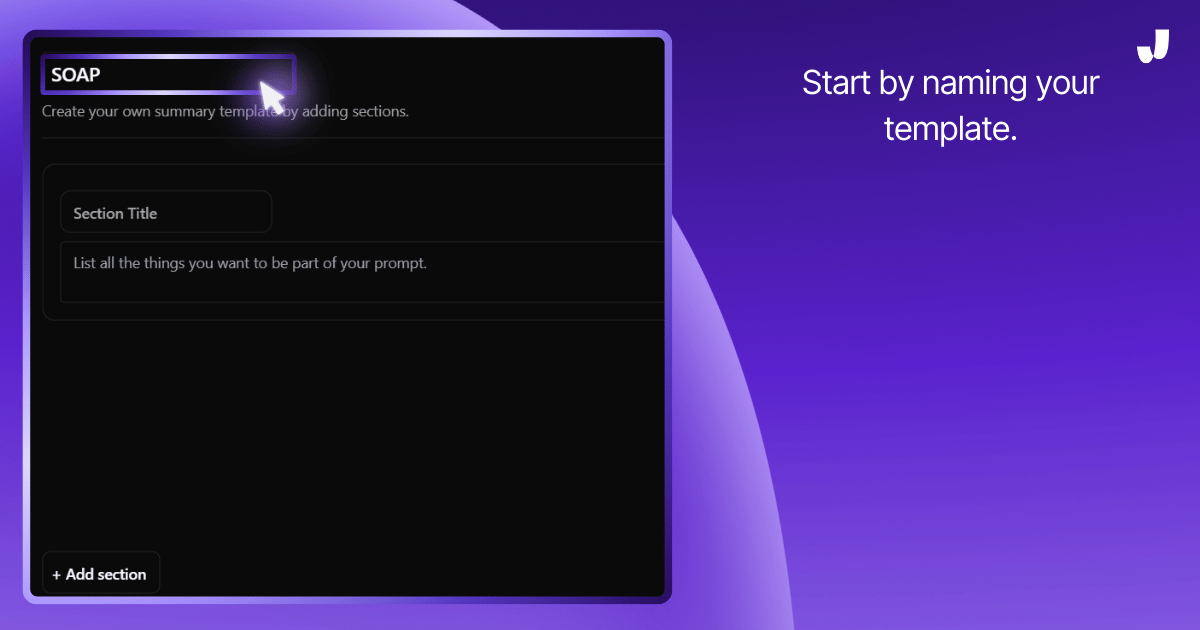
- Section Title: Then start adding a title for the first section, like "Subjective" for SOAP notes.
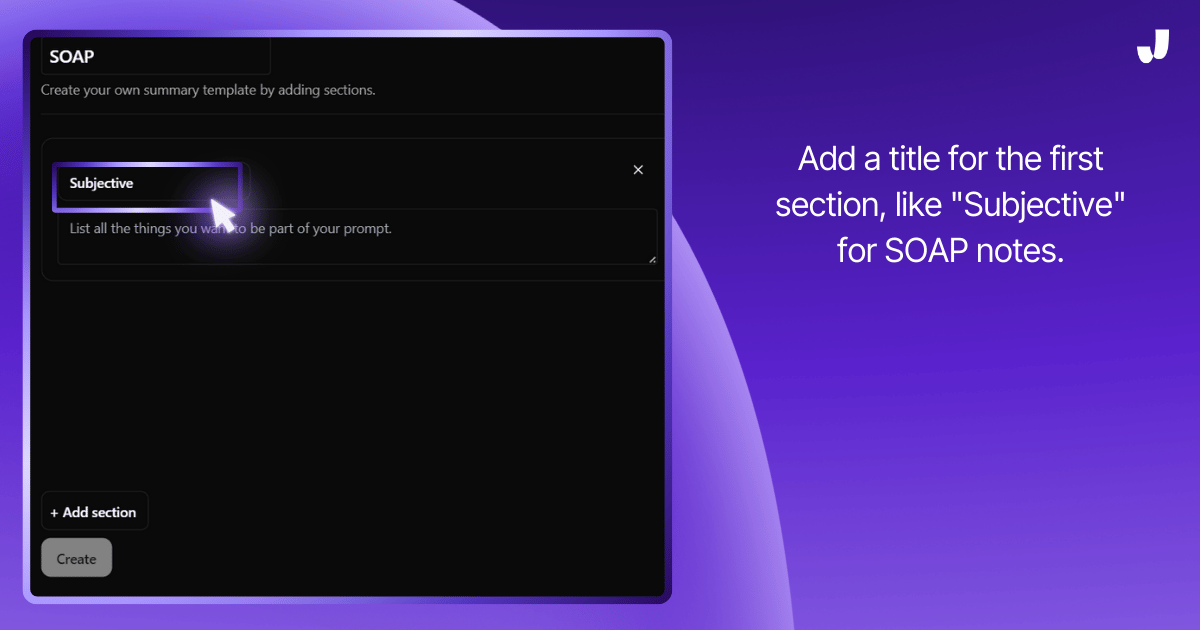
- Content: In the prompt area, write down what you want Jamie to capture for this section.
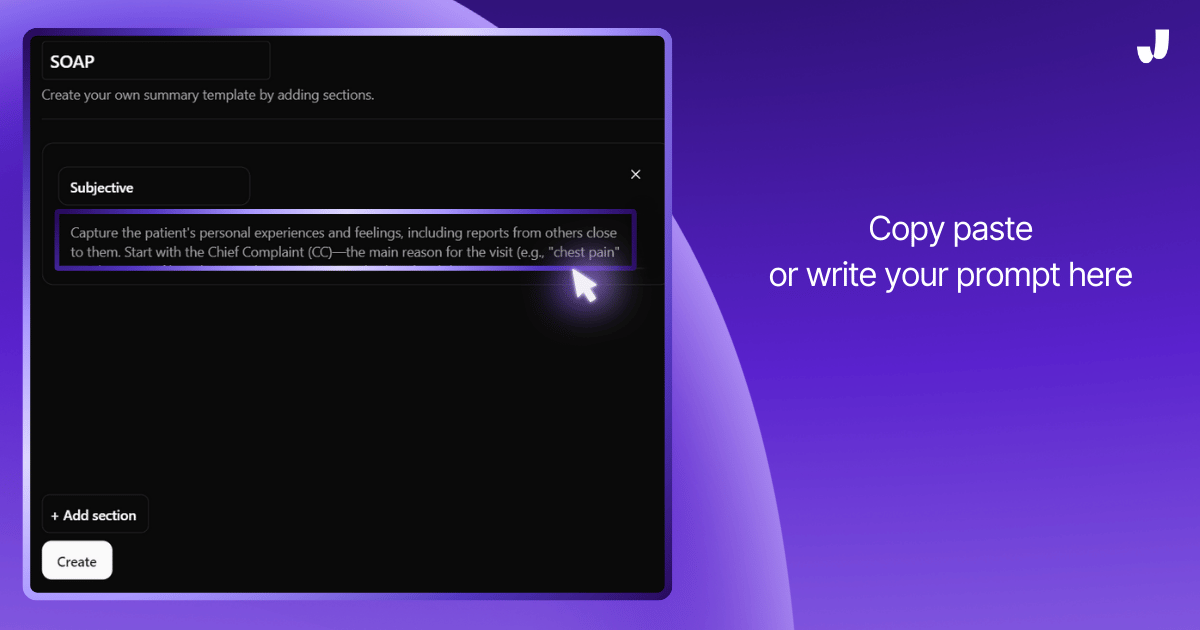
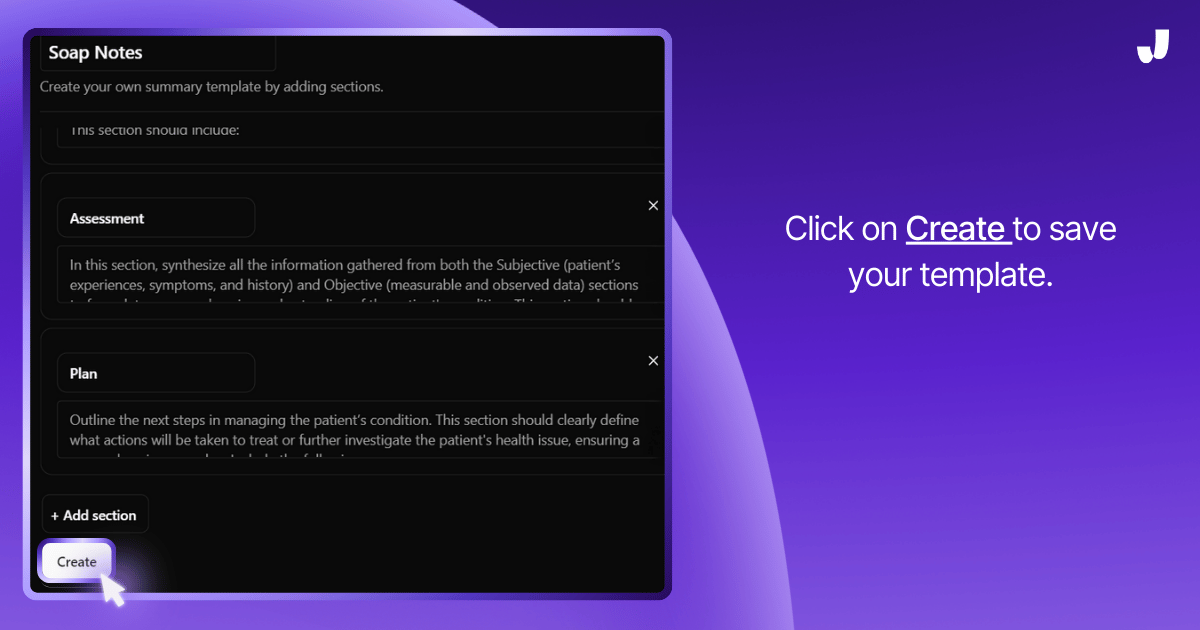
- Add More Sections: Click + Add section to create additional sections like "Objective," "Assessment," and "Plan," filling out the prompts as needed.
Step 7: Save the Template
Once you’ve finished customizing your template,
- Save the Template: Click on Create to save your template.
Step 8: Start Your Meeting or Session And Apply the Template
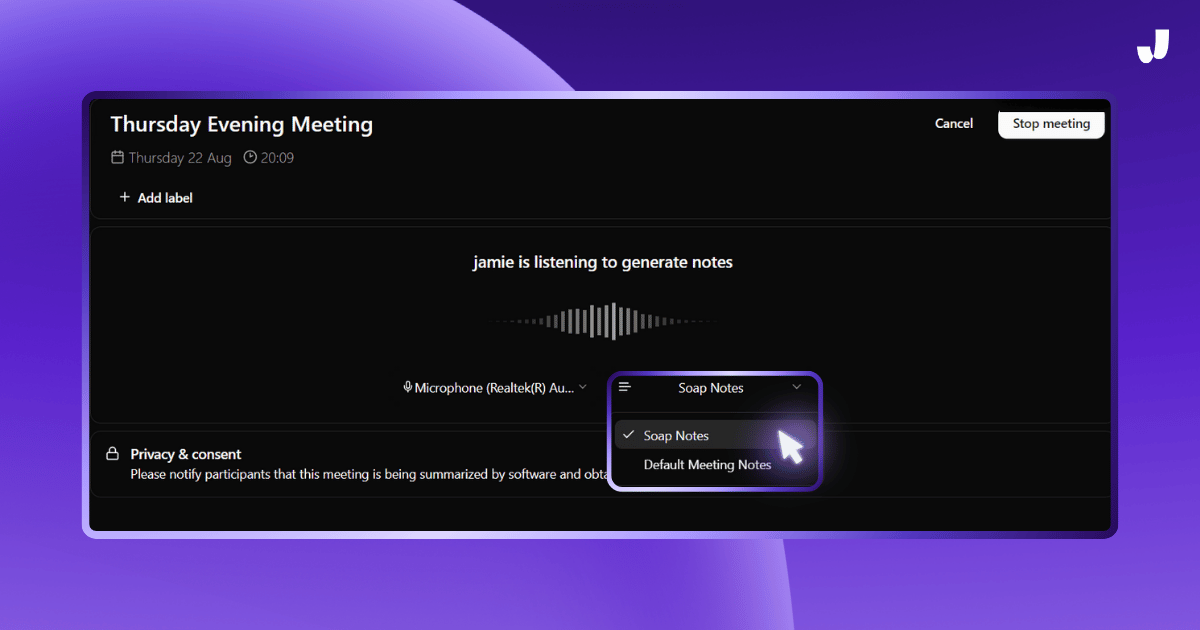
Now you’re ready to start your meeting or session.
- Record the session. Let Jamie listen in during your session or meeting. Jamie will automatically capture everything it hears.
- Apply the template: When you start your meeting, you will get the drop down menu to select the preferred template as below.
- Sit Back and Relax: Jamie will use your customized template to generate detailed progress notes based on the meeting or session.
Step 9: Review and Edit Notes
After the session,
- Check the Notes: Once Jamie has finished processing, it will generate the progress notes using your template.
- Make Any Edits: Review the notes and make any adjustments if needed. Jamie’s notes are detailed, but you have the final say!
Step 10: Save and Share Your Notes
Finally, when you’re satisfied with the notes:
- Save the Notes: Save the final version to your records.
- Share: You can easily share the notes with others via email or a secure URL, ensuring everyone involved is up-to-date.
SOAP Note Example with Jamie
Here's a real-life example of a doctor-patient progress note that Jamie accurately captured.
Executive Summary:
- Patient presented with severe chest pain (8/10) for three days, described as stabbing and centered in the chest, with associated shortness of breath.
- Diagnostic plan includes EKG, blood tests, and possible chest x-ray to rule out heart issues, with differential diagnosis of costochondritis or potential cardiac problems.
- Treatment involves anti-inflammatory medication, referral to a cardiologist, rest instructions, and guidelines for seeking emergency care if symptoms worsen.
Meeting Notes:
Patient Presentation
- Patient presented with chest pain that started three days ago
- Patient reported still having chest pain at the time of the consultation
Symptoms Assessment
Chest Pain Characteristics
- Location: Center of the chest
- Nature: Described as a stabbing pain
- Duration: 20 to 30 minutes each episode
- Intensity: Rated as 8 out of 10 on a pain scale
- Factors affecting pain:
- Worsens with deep breaths or movement
- Improves with rest
- No specific time of day when pain is worse
Associated Symptoms
- Patient reported feeling short of breath
- No lightheadedness, feeling of passing out, sweating, or nausea
- No pain radiating to back or arms
Physical Examination
Vital Signs
- Blood pressure: 120/80 mmHg
- Heart rate: 78 beats per minute
- Respiratory rate: 16 breaths per minute
- Oxygen saturation: 98%
Chest Examination
- Palpation: No additional pain caused by pressing on the chest
- Auscultation: Heart and lung sounds normal, no murmurs or wheezing
Medical History
- Patient mentioned having anxiety, which is a significant aspect of their mental health history.
- No current prescription medications have been reported
Differential Diagnosis
- Costochondritis (inflammation of the cartilage in the chest wall)
- Possible heart issues (to be ruled out)
Diagnostic Plan
- EKG (electrocardiogram)
- Blood tests to check heart function
- Possible chest x-ray, depending on initial test results
Treatment Plan
Medication
- Anti-inflammatory medication is prescribed for pain relief. Patients who occasionally use otc sleep aids to address their sleep disturbances often find these aids beneficial as part of a broader treatment plan for anxiety and depression, improving sleep quality and overall well-being.
Referrals
- Referral to a cardiologist for further evaluation
Follow-up Instructions
Activity Restrictions
- Avoid heavy lifting and strenuous activity
- Rest as much as possible
- Try to stay calm, as stress and anxiety can worsen chest pain. Developing effective coping strategies, such as cognitive-behavioral therapy (CBT) and seeking social support, can help manage symptoms of anxiety and depression.
Emergency Situations
- Doctor instructed Patient to go to the emergency room immediately if:
- Pain worsens
- Shortness of breath develops
What Are Progress Notes and Why Are They Important?
Progress notes are notes that doctors, therapists, or other healthcare professionals write down to monitor the progress of their patients over time.
They’re extremely important because these notes become the core memory for professionals because they help them remember what happened in previous sessions and help diagnose what to do in the next session with their patients or clients.
Mental health professionals, such as psychiatrists, psychotherapists, and clinical social workers, utilize these notes to maintain organized and accessible patient records, aiding in understanding the patient's status and treatment plans.
What Are Soap Notes?
SOAP notes are used by healthcare providers to document patient information. It was developed almost 50 years ago by Larry Weed.
These notes help doctors and nurses understand a patient’s physical or mental status and foster communication between different healthcare professionals.
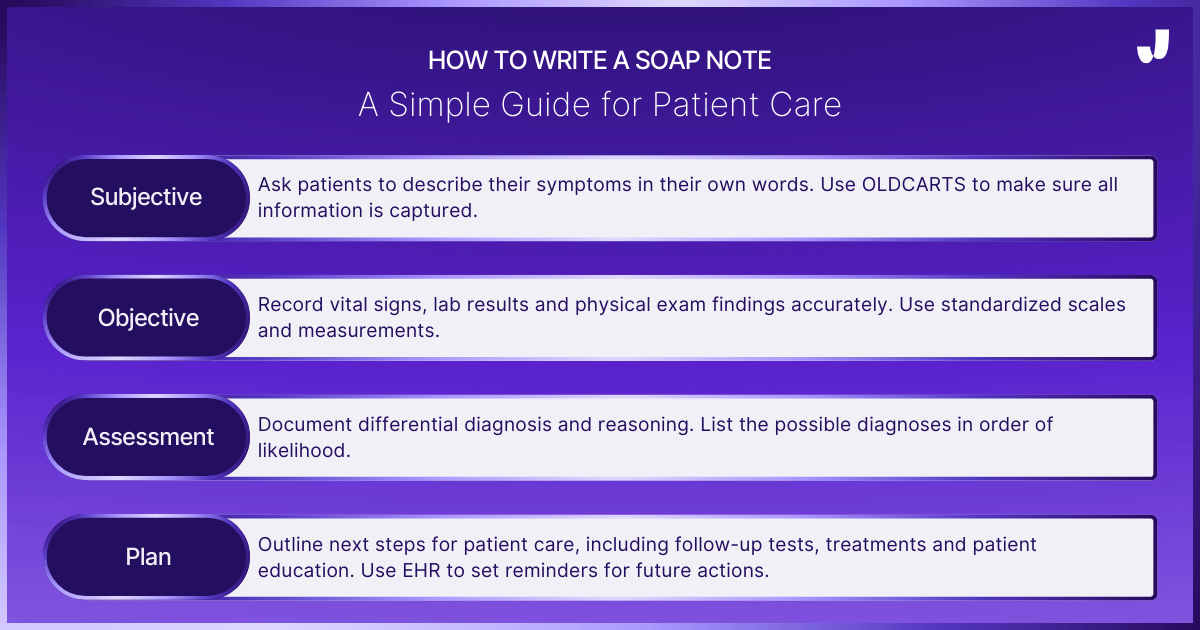
The SOAP note is divided into 4 sections:
- Subjective,
- Objective,
- Assessment, and,
- Plan.
Subjective
This section captures the patient’s
- Personal experiences,
- Feelings or what others close to them report.
For example, if a patient says, "I have a headache," that information is recorded here.
This section usually starts with the patient’s main reason for visiting, known as the Chief Complaint (CC).
It could be something like "chest pain" or "shortness of breath."
The patient describes:
- When the problem started,
- Where it hurts,
- How long it’s been hurting and,
- What makes it better or worse.
This detailed description is organized using the acronym "OLDCARTS," Each letter in OLDCARTS stands for a part of the symptom the healthcare provider needs to know to better understand the problem and make a diagnosis.
Here’s what each letter means:
- O - Onset: When did this start?
- L - Location: Where is it?
- D - Duration: How long has it been going on?
- C - Characterization: How does the patient describe it?
- A - Alleviating and Aggravating Factors: What makes it better or worse?
- R - Radiation: Does it go to other parts of the body?
- T - Temporal Factors: Is it worse or better at certain times of the day?
- S - Severity: How bad is it on a scale of 1 to 10, with 10 being the worst?
How it Works: Using OLDCARTS, the provider gets all the information about the patient’s symptoms. By following this structured approach, the patient’s story becomes a clear and complete picture so the healthcare provider can figure out what’s wrong and how to fix it. (Source)
Objective
This section is about the factual, measurable information gathered during the patient’s visit.
It includes;
- Vital signs (blood pressure, heart rate),
- Physical exam findings,
- And lab tests or imaging results.
Unlike the subjective section, which is based on what the patient says, this section is based on what the healthcare provider observes or measures. (Source)
Assessment
Here, the healthcare provider combines all the information from the subjective and objective sections to determine what’s wrong with the patient.
They list possible diagnoses and explain their reasoning.
This should include:
- Differential Diagnoses: identifying possible conditions causing symptoms.
- Clinical Reasoning: thinking through patient care decisions.
- Prioritization: deciding what to treat first based on urgency.
Plan
This final section outlines what will be done next to treat or further investigate the patient’s condition.
It includes;
- Additional tests,
- Medications,
- Referrals to specialists and,
- Any advice or education given to the patient.
This section helps future healthcare providers understand what has been done and what needs to happen next. (Source)
It's Your Turn To Generate Accurate Progress Notes With Jamie
Jamie has shown that automating progress notes is not just possible but essential for modern healthcare professionals.
Remember that simple idea—to take the load off healthcare professionals?
Jamie has turned that idea into reality. Now it’s your turn to benefit—download Jamie today and let it handle the paperwork, so you can focus on what truly matters: your patients.
FAQs: AI Progress Notes Generator
Can AI Progress Note Generators Understand and Use Medical Terminology Accurately?
Yes, advanced AI progress note generators like Jamie can be trained to understand and use medical terminology accurately. Jamie allows you to customize templates and train the AI to recognize specific terms relevant to your practice. This ensures that the generated notes are not only accurate but also tailored to your needs.
How Does AI Ensure the Privacy and Security of Patient Data?
AI tools like Jamie prioritize data security by implementing encryption and ensuring compliance with privacy regulations such as GDPR. Additionally, Jamie deletes audio files after transcription, ensuring that no sensitive data is stored unnecessarily.
Can AI Handle Different Note Formats Like SOAP, DAP, or BIRP?
Yes, AI tools like Jamie are versatile and can handle multiple note formats including SOAP, DAP, BIRP, and more. You can create and customize templates for any format you prefer, making it easier to generate structured and comprehensive notes.
What Are the Common Challenges in Using AI for Progress Notes?
One of the main challenges is ensuring the accuracy of the generated notes, especially in noisy environments or with complex cases. However, with tools like Jamie, which are designed to adapt to your workflow and medical terminology, these challenges can be minimized.
Are There Free AI Tools Available for Progress Note Generation?
Yes, there are free options like Jamie’s basic plan, which offers a limited number of meeting credits per month. This allows you to explore AI-generated notes without a financial commitment.
Sanduni Yureka is a Growth Content Editor at Jamie, known for driving a 10x increase in website traffic for clients across Singapore, the U.S., and Germany. With an LLB Honors degree and a background in law, Sanduni transitioned from aspiring lawyer to digital marketing expert during the 2019 lockdown. She now specializes in crafting high-impact SEO strategies for AI-powered SaaS companies, particularly those using large language models (LLMs). When she’s not binge-watching true crime shows, Sanduni is obsessed with studying everything SEO.
Read more
3 min to save 1000 hours
Download Jamie now
Start your meeting
Super-charge your workday




.png)
.png)


.-p-500.png)


